Radiation therapy, or radiotherapy, is a treatment involving the use of high-energy sources to kill cancer cells. Radiation may come from a machine outside the body (external radiation therapy) or it may come from radioactive materials (radioisotopes) placed directly into or near the area where the cancer cells are found (internal radiation therapy, or brachytherapy).
There are many options of radiation therapy as well as many chemotherapy agents. However, not all radiotherapy options are available to all medical centers, nor are all options applicable for treating skull base diseases.
In addition to destroying cancer cells, radiation to the head and neck area can harm normal cells, including cells in the mouth and oropharynx. Patients receiving radiation therapy to the head and neck area will be at risk for developing certain problems such as dry mouth, malnutrition, and dental problems. Some people experience other problems in the head and neck area such as hardening of the tissues (fibrosis) and thyroid malfunction. However, each person is different – each patient may respond differently to treatment. You may experience differences in type and degree of side effects of treatment.
Fractional Schedules
In radiation therapy, the total dose of radiation is divided into several smaller, equal doses delivered over a period of several days or weeks, also known as fractionation. The radiation oncologist can choose from several different radiation schedules discussed below:
Standard Radiation Therapy is usually given as an outpatient, five days a week for a given period of time. Radiation has the advantage of avoiding surgical risk, possibly preserving organs and therefore organ function, as well as being able to easily treat large areas of tumors or potential tumor involvement that might otherwise be difficult to reach with surgery and result in greater post-operative defect and dysfunction.
Accelerated Fractionation is treatment with multiple daily fractions of approximately standard size to about the same total dose, but is given in a shorter overall time.
Hyperfractionated Radiation Therapy is the use of multiple radiation fractions (doses) per day of smaller than conventional size but to a higher total dose, with little or no change in overall treatment time. The rationale for this type of therapy is that it allows less time in between treatments for the tumor cells to recover from the radiation damage. However, there is a greater risk of acute radiation-associated side effects with this form of treatment.
Types of Radiation Therapy
Brachytherapy or Radiation Implant Therapy is the actual placement of radiation sources into the tumor or tumor bed site. In this way, radiation does not have to travel through healthy tissue in order to reach the cancer. Radiation to healthy tissue, as well as side effects, is minimized. Brachytherapy can utilize high doses of radiation to the tumor bed, thereby increasing the rate of cure. Side effects associated with brachytherapy include soft tissue complications, problems with wound healing, development of ulcers, and delayed mucositis.
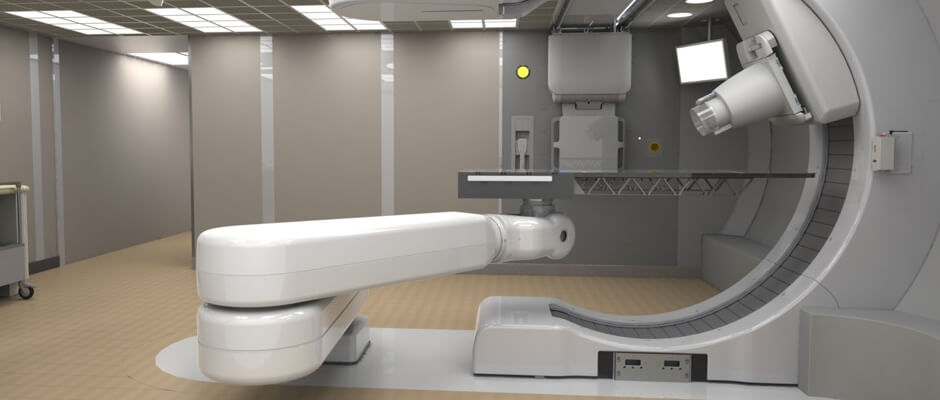
External Radiation Therapy
The following treatments deliver radiation treatment using an external beam of radiation directed at the tumor. The radiation can be administered with machines that vary accordingly to the energy produced and the ionizing particles delivered. The higher the energy produced, the grater the depth of penetration of the radiation beam.
Conformal Radiation is a technique that uses data from CT scans and/or MRI scans to crate a three-dimensional picture of a tumor so that radiation beams conform (shape exactly) to a target. This type of treatment allows for higher doses of radiation to be delivered directly to the tumor, while lessening the effects on adjacent normal tissues. Conformal radiation therapy requires the use of special equipment.
Intensity Modulated Radiation Therapy (IMRT) is a form of conformal radiation that allows for more shaping of the radiation distribution and doses by varying the intensity of the radiation beams. Increased conformality leads to better sparing of normal tissues. It is becoming increasingly more available at medical facilities.
Tomotherapy combines treatment planning, patient positioning and treatment delivery into a single system. This allows doctors to perform a special CT scan just before each treatment, and then adjust the patient's position if necessary to ensure that the radiation is delivered in a highly precise fashion to the tumor without exposing healthy tissue to unnecessary radiation. Tomotherapy delivers radiation using a helical 360 degree loop pattern, traveling in multiple circles around the patient who lies on a movable treatment couch that guides the patient into the treatment unit.
3D Stereotactic Radiation is a form of conformal radiation that delivers highly focused radiation to a tumor using a rigid head immobilization technique and three-dimensional treatment planning and dose delivery. Traditionally, the planning of radiation treatments has been done in two dimensions (width and height). Three-dimensional conformal radiation therapy uses computer technology to allow doctors to more precisely target a tumor with radiation beams (using width, height, and depth).
Fast Neutron Therapy uses neutrons that typically deposit more energy to tissues than conventional x-rays or electrons used in radiotherapy. Because of the higher energy neutron deposit, certain tumors, including salivary gland tumors, appear more responsive to neutron radiotherapy than to standard radiotherapy. However, in depositing high energy to the tumors, neutrons also deposit more energy to normal tissues adjacent to tumors, resulting in greater side effects than those of standard radiation therapy. Hence, neutron radiotherapy is restricted to those situations in which such treatment may yield a therapeutic advantage over conventional radiation.
There are only three neutron treatment facilities in the United States where neutron therapy is available for the treatment of salivary gland tumors: the University of Washington Medical Center in Seattle, Washington; Harper University Hospital in Detroit, Michigan; and the Fermilab National Laboratory in Batavia, Illinois.
Proton Therapy is a form of external-beam radiation treatment. Proton beam radiotherapy (PBRT) uses protons – positively charged subatomic particles – that are much more powerful than electrons used in conventional radiation therapy to fight cancer. The proton dose of radiation can be controlled by the radiation oncologist to an exact shape and depth within the body. Because proton beams have less scatter than other sources of energy, proton beam radiotherapy can be used to escalate radiation dose to designated tissue, while minimizing damage to adjacent healthy tissue.
Proton Therapy is available at Loma Linda University Medical Center in California, the Midwest Proton Radiotherapy Institute at Indiana University, the Northeast Proton Therapy Center at Massachusetts General Hospital in Boston and the MD Anderson Proton Therapy Center, Texas Medical Center in Houston, Texas.
